Description
Melanoma is a form of skin cancer that begins in the cells that make melanin, the pigment which gives skin its color. Melanoma can form anywhere on the skin, but most commonly starts on the chest or back in men, and on the legs in women. They are more common in individuals with lighter skin tones.
Melanoma is a rarer form of skin cancer, but it is among the most deadly, and is likely to spread quickly. Average age at diagnosis is 66, though close to 5% of melanomas are found in individuals under the age of 35.[1]
Melanoma may not cause obvious symptoms other than its own appearance on the skin (usually as a new abnormal mole, bump, or discoloration). When determining whether a spot on the skin may be melanoma, individuals are encouraged to use the “ABCDE” test:
- Asymmetry - when one half of a mole or birthmark is not a mirror image of the other half
- Border - the edges are irregular, notched/jagged, or blurred
- Color - the color is not uniform throughout the spot or mole (this could mean different shades of brown or black, or patches of pink, red, white, or blue)
- Diameter - the spot is larger than a pencil eraser from edge to edge (about 6 mm across)
- Evolving - an existing mole or lesion appears to be changing in size, shape, or color
These metrics may not mean a given spot is melanoma, and some melanomas do not show these signs. Any new spots on the skin should be examined by a doctor. In addition to the above visual markers, melanomas may cause:
- Sores that won’t heal
- Pigment spread outside of a previously existing mole / into surrounding skin
- Redness or swelling
- Itching, pain, or tenderness
- Scaling, oozing, or bleeding on the skin or the surface of a mole
Melanoma can also appear inside the mouth, in the iris (the colored portion of the eye), or beneath finger- or toenails. If you spot changes or new discolorations in these portions of your body, you should speak about them with your doctor.
Different forms of melanoma are characterized by distinct features and biological behaviors:
- Superficial spreading melanoma: This form of melanoma begins as a tumor that grows outward on the skin’s surface, sometimes starting in an existing mole. They may be noticed as a dark spot that is growing or changing shape. About 70% of melanomas are of this type.
- Lentigo maligna melanoma: Most common in older people, lentigo maligna melanomas usually appear as irregularly-shaped brown or tan spots in areas with significant sun exposure (like the face or arms). They tend to grow slowly.
- Nodular melanoma: In nodular melanoma, tumors appear as a distinct raised bump which can be brown, black, pink, or red in color. They penetrate deeper layers of the skin more quickly than other forms of melanoma, which means they’re often more advanced when they’re diagnosed.
- Acral melanoma: These melanomas appear on portions of the body that don’t get much sun exposure, like the palms, the soles of the feet, or the skin beneath finger- or toenails. These are much more common in individuals with darker skin tones.[2]
There are also benign growths that can form on the skin and which may resemble melanoma. Depending on location and size, as well as your personal history, your doctor may suggest removal as the safest route.
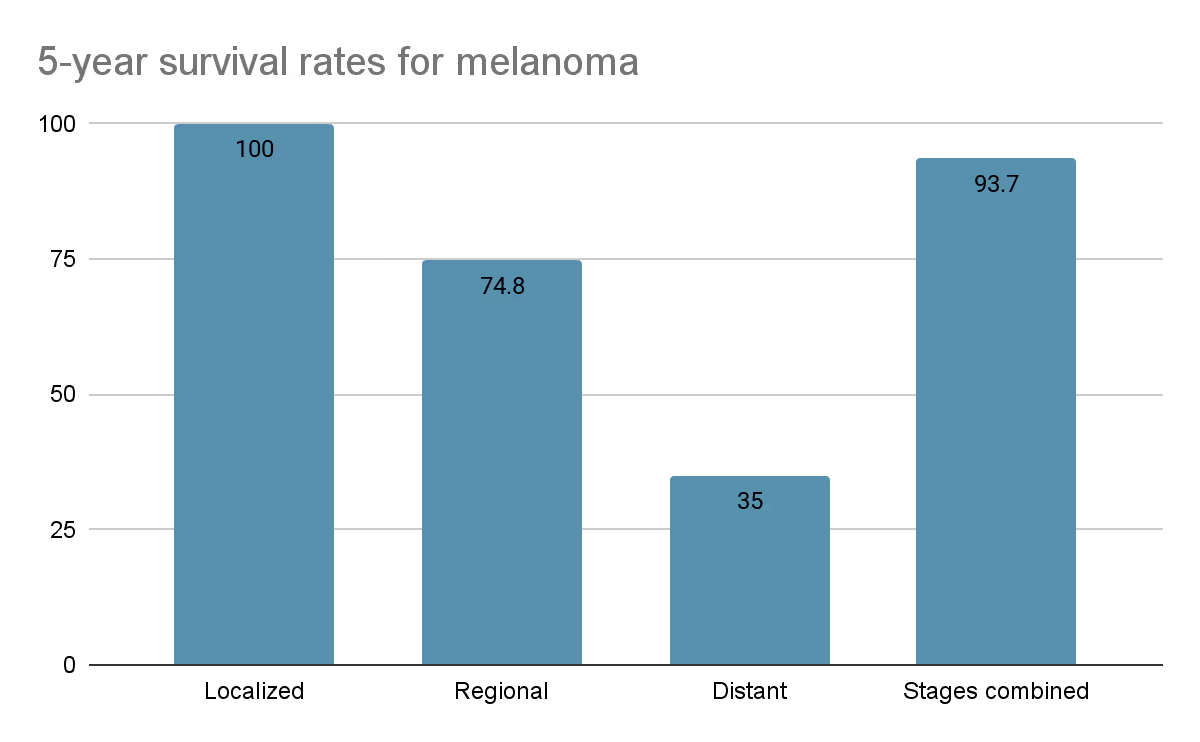
Melanoma survival rates are based on how far the cancer has spread:
- Localized: There is no sign the cancer has spread from its origin point.
- Regional: The cancer has spread to nearby structures or lymph nodes
- Distant: The cancer has spread to distant parts of the body, such as the liver or bones.
The 5-year survival rate for each stage is shown below:
Incidence
Below is the overall incidence of melanoma by age group:


Risk Factors
There are several confirmed risk factors that contribute to an individual’s risk for melanoma:
- Childhood sunburn(s)[3]: Just one blistering sunburn in childhood can more than double your risk of developing melanoma later in life. The more sunburns you experience, especially in childhood, the higher your risk.
- Fair skin / skin that burns easily / freckles / red or blond hair: Skin tone, eye color, and hair color are all regulated by melanin, and individuals with lower amounts of melanin are at higher risk for developing melanoma. Fair skin, burning or freckling easily, and light colored hair are all indicators of lower melanin.
- Number of moles: Moles are usually harmless in themselves, but are functionally a benign skin tumor[4]. The more moles you have on your body, the higher your risk for melanoma.
- Health conditions[5][6]:
- Endometriosis: A large Scottish study showed a significant increase in melanoma risk for women with endometriosis compared to those without the condition. The reasons behind this link aren’t fully understood yet.
- Type 2 diabetes: Individuals with type 2 diabetes may be at higher risk for malignant melanoma, though more study is needed to confirm this link.
- Genetic conditions: Some melanomas are likely caused by inherited genetic conditions, such as BRCA2 mutation (which increases melanoma risk for both men and women).
- Family history of melanoma: Even without specific inherited genetic conditions, a family history of melanoma corresponds to a higher overall risk of developing the disease.
- Time spent outside: Ultraviolet (UV) rays are the main cause of skin damage, and can cause the DNA in skin cells to mutate. Significant exposure to the sun–particularly in the summer when the proportion of UV rays is higher–is a major risk factor for melanoma.
- Use of indoor tanning beds[7]: Tanning beds emit UV rays in much higher concentrations than are found in sunlight, and they mostly emit UVA rays, which penetrate deeper into the skin. In one study, using a tanning bed before the age of 35 was associated with a 75% increase in melanoma risk.
- Occupational radiation exposure: Working in a job that exposes you to significant amounts of ionizing radiation[8] (learn more about ionizing vs. non-ionizing radiation) can increase your risk of melanoma. Medical workers, particularly those working frequently with CT scans or X-rays, nuclear plant workers, miners, and air-travel employees whose jobs require extended flight time are all at risk via this form of exposure.
- Use of oral contraceptives: Several studies have shown a link between use of oral contraceptives and melanoma risk.
Protective Factors
Some factors have been shown to have protective effects against melanoma:
- Regular sunscreen use: Regular sunscreen use, both in childhood and consistently throughout one’s life, has a strong protective effect against melanoma[9]. The American Cancer Society recommends broad spectrum sunscreen (which offers protection against both UVA and UVB rays) of at least SPF 30 strength in order to protect yourself.[10]
- Tea consumption: Green tea and black tea are rich in polyphenols like catechins which have strong antioxidant properties. Antioxidants help neutralize free radicals that can damage cells and lead to cancer, including melanoma[11]. The polyphenols in tea also exhibit anti-inflammatory effects, which can reduce chronic inflammation, a known risk factor for various types of cancer. Some studies suggest that compounds in tea can inhibit the growth of cancer cells and promote apoptosis (programmed cell death), potentially reducing the risk of cancer development and progression
Screening
Early detection of melanoma has a dramatic impact on prognosis. The 5-year survival rate for localized melanoma is 100%, but drops to just 35% once the cancer has spread to distant parts of the body.
Depending on your age and risk factors, the optimal melanoma screening will vary:
- Regular physical/dermatological exams: During thorough physicals or dermatological screenings, your doctor will look for any spots or moles that show features of possible melanoma, and will also weigh any symptoms you’re experiencing. Regular visits will allow your doctor to track any changes to existing moles or spots that might give cause for concern.
- Dermascopy: In this form of screening your doctor will use a dermatoscope (an instrument which can magnify and illuminate small sections of the skin) to more closely examine any suspicious spots or skin patches. This instrument can also capture digital imagery which can be computer-analyzed to determine whether further tests are needed.
- Reflectance conscopal microscopy (RCM): Similarly to dermascopy, this screening technique allows a doctor to get a more detailed view of a small section of the skin, via low-powered lasers trained on suspicious areas. This is especially useful for suspicious moles that might otherwise require biopsy.
- Adhesive patch testing: In this test a sticky patch is placed over a suspicious section of skin, and cells that adhere to it upon removal are tested for genetic signatures of melanoma.
- Biopsy: There are multiple forms of biopsy that remove some or all of a suspicious portion of skin for further testing. Local anesthetic numbs the area in question, and the removed sample is sent to a laboratory for further analysis. Usually there will be a small scar with this form of testing.
- Liquid biopsy: Liquid biopsy is an investigational cancer-detection technique which looks for DNA fragments in the blood to determine whether cancer is present. Though still in its infancy, this technology is promising, particularly in screening for hard-to-detect cancers or cancers whose symptoms are minimal or tend to appear only after they’ve spread. Melanoma is one of many cancers which can be screened for via this method.










.svg)



